Understanding Coronary Artery Disease: A Comprehensive Guide
Understanding Coronary Artery Disease: A Comprehensive Guide, also known as coronary heart disease (CHD), is one of the most prevalent and deadly conditions affecting millions of people worldwide. It refers to the narrowing or blockage of the coronary arteries due to a buildup of plaque, which restricts blood flow to the heart. This reduction in blood flow can lead to chest pain, heart attacks, and other severe cardiovascular issues. The good news is that CAD can often be prevented or managed through lifestyle changes, medication, and, in some cases, surgical interventions.
What is Coronary Artery Disease?
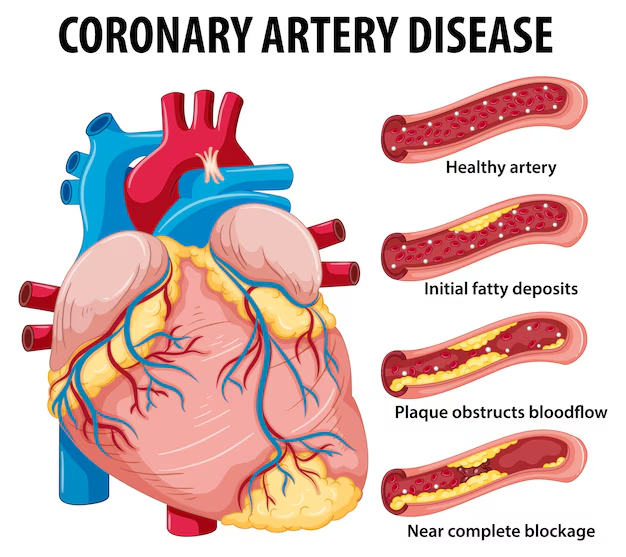
Coronary artery disease occurs when the coronary arteries, which are responsible for supplying oxygen-rich blood to the heart muscle, become narrowed or blocked. The main cause of this blockage is atherosclerosis, a condition where fatty deposits, or plaques, build up in the walls of arteries.
The heart requires a constant supply of oxygenated blood to function properly. When blood flow to the heart muscle is restricted, it can lead to chest pain (angina), shortness of breath, fatigue, and even heart attacks. In some cases, CAD can progress to heart failure, a condition where the heart is unable to pump blood effectively to meet the body’s needs.
Causes of Coronary Artery Disease
The primary cause of coronary artery disease is the accumulation of plaques in the coronary arteries. This process, known as atherosclerosis, occurs over many years and is influenced by various risk factors. The exact causes of atherosclerosis are not entirely understood, but several factors contribute to the development of CAD:
- Unhealthy Diet: A diet high in saturated fats, trans fats, cholesterol, and processed foods can lead to an increase in low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol. Elevated levels of LDL cholesterol can contribute to plaque formation in the arteries.
- High Blood Pressure (Hypertension): High blood pressure can damage the inner lining of the arteries, making them more susceptible to plaque buildup. The increased pressure also forces the heart to work harder, which can strain the cardiovascular system over time.
- Smoking: Smoking is one of the leading causes of cardiovascular disease. It damages the blood vessels, increases blood pressure, and lowers the levels of high-density lipoprotein (HDL) cholesterol, also known as “good” cholesterol. This combination accelerates the development of CAD.
- High Cholesterol: Elevated cholesterol levels, especially high levels of LDL cholesterol, increase the risk of plaque formation in the arteries. HDL cholesterol, on the other hand, helps remove cholesterol from the blood vessels and reduces the risk of CAD.
- Diabetes: People with diabetes, particularly those with poorly controlled blood sugar levels, are at a higher risk of developing CAD. High blood sugar levels can damage the blood vessels and contribute to plaque buildup.
- Physical Inactivity: A lack of physical activity is a major risk factor for coronary artery disease. Regular exercise helps to maintain healthy blood pressure and cholesterol levels, while physical inactivity contributes to weight gain, hypertension, and poor cardiovascular health.
- Age and Gender: As we age, the risk of CAD increases. Men are generally at higher risk at an earlier age, but after menopause, women’s risk of CAD rises significantly, often catching up to that of men.
- Chronic Stress: Long-term stress can contribute to high blood pressure and other unhealthy behaviors, such as overeating or smoking, that increase the risk of CAD.
Symptoms of Coronary Artery Disease
In the early stages of CAD, many individuals do not experience any noticeable symptoms. Some common signs of CAD include:
- Angina (Chest Pain or Discomfort): Angina is the most common symptom of CAD. The pain may radiate to the shoulders, arms, neck, jaw, or back. Angina typically occurs during physical activity or emotional stress, when the heart requires more oxygen than it is receiving due to narrowed arteries.
- Shortness of Breath: When the heart cannot pump blood efficiently, fluid may accumulate in the lungs, leading to shortness of breath. This can occur during physical exertion or even at rest, depending on the severity of the disease.
- Fatigue and Weakness: As blood flow to the heart decreases, the heart may not be able to pump blood effectively to other organs and tissues in the body. This can result in feelings of fatigue, weakness, and decreased exercise tolerance.
- Dizziness or Lightheadedness: In more severe cases of CAD, individuals may experience dizziness, lightheadedness, or even fainting due to reduced blood flow to the brain.
- Heart Attack (Myocardial Infarction): A complete blockage of a coronary artery can cause a heart attack. Symptoms of a heart attack include sudden, severe chest pain, shortness of breath, nausea, sweating, and lightheadedness. A heart attack is a medical emergency and requires immediate treatment.
- Arrhythmias: Some individuals with CAD may experience irregular heartbeats or palpitations, which can cause a sensation of fluttering or rapid heartbeats.
It is important to note that the symptoms of CAD can vary between individuals, and some people may experience atypical symptoms, particularly women, elderly individuals, and people with diabetes.
Diagnosis of Coronary Artery Disease
If CAD is suspected, healthcare providers will typically perform several tests to confirm the diagnosis and determine the extent of the disease. Common diagnostic tests include:
- Physical Examination and Medical History: The doctor will begin by reviewing your medical history, risk factors, and lifestyle habits. A physical examination will assess your blood pressure, heart sounds, and overall health.
- Electrocardiogram (ECG or EKG): An ECG measures the electrical activity of the heart and can help identify signs of a heart attack, arrhythmias, or insufficient blood flow to the heart.
- Stress Test: A stress test involves exercising on a treadmill or stationary bike while the heart is monitored. This test helps assess how well the heart responds to physical activity and can reveal any underlying CAD or arrhythmias.
- Echocardiogram: This imaging test uses sound waves to create images of the heart. An echocardiogram can help assess the heart’s function, check for areas of reduced blood flow, and detect valve issues.
- Coronary Angiography: This is the most definitive test for diagnosing CAD. A catheter is inserted into a blood vessel, and a dye is injected into the coronary arteries. X-ray imaging is then used to identify blockages or narrowing of the arteries.
- CT or MRI Scans: Non-invasive imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) can help assess the coronary arteries and detect signs of CAD.
Treatment of Coronary Artery Disease
The treatment for coronary artery disease depends on the severity of the condition and the symptoms experienced. Treatment options include lifestyle changes, medications, and in some cases, surgical interventions.
1. Lifestyle Changes
Adopting a heart-healthy lifestyle is the first step in managing CAD. Some key lifestyle modifications include:
- Healthy Diet: Eating a balanced diet that is low in saturated fats, trans fats, and cholesterol. Include plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats (e.g., omega-3 fatty acids).
- Exercise: Engaging in regular physical activity, such as 30 minutes of moderate exercise most days of the week, can help improve heart health.
- Weight Management: Maintaining a healthy weight can help lower the risk of CAD and reduce the strain on the heart.
- Quit Smoking: Stopping smoking is one of the most important steps to reduce the risk of heart disease.
- Stress Management: Managing stress through relaxation techniques, mindfulness, and hobbies can help reduce the burden on the heart.
2. Medications
- Statins to lower cholesterol levels.
- Aspirin or other antiplatelet drugs to reduce the risk of blood clot formation.
- Beta-blockers to control blood pressure and reduce the heart’s workload.
- ACE inhibitors to relax blood vessels and lower blood pressure.
3. Surgical Interventions
In more severe cases of CAD, surgical procedures may be necessary to restore blood flow to the heart:
- Angioplasty and Stenting: A balloon is used to open up blocked arteries, and a stent is placed to keep the artery open.
- Coronary Artery Bypass Grafting (CABG): This procedure involves taking a healthy blood vessel from another part of the body and using it to bypass blocked arteries, restoring blood flow to the heart.
Prevention of Coronary Artery Disease
Prevention is key to reducing the risk of coronary artery disease. Steps to prevent CAD include:
- Eat a heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats.
- Exercise regularly to maintain a healthy weight and reduce the risk of CAD.
- Avoid smoking and limit alcohol consumption.
- Monitor blood pressure and cholesterol levels regularly.
- Manage stress through relaxation techniques and healthy coping mechanisms.
- Get regular check-ups to detect and manage risk factors like high blood pressure, high cholesterol, and diabetes.
Conclusion
Coronary artery disease is a serious and potentially life-threatening condition, but it is also preventable and manageable. By understanding its causes, recognizing the symptoms, and taking steps to adopt a healthy lifestyle, you can significantly reduce your risk of developing CAD. Early diagnosis and appropriate treatment are crucial for managing the disease and improving quality of life. Taking care of your heart today can ensure a healthier future for years to come.


Leave a reply